Reviewed by Sahil Chopra, MD, and Stacey Gunn, MD.
Research by Savit Malhotra and Theresa Do.
Introduction
This week, we will take a look at another dermatological condition, psoriasis, and its relationship to sleep. Psoriasis is a lifelong disease that can impact the quality of life and, importantly, the quality of sleep for those affected. Globally, 125 million people had psoriasis in 2019, according to the National Psoriasis Foundation.[1] In the United States alone, psoriasis impacts more than 8 million adults, and an estimated 600,000 adults live with undiagnosed cases.[1] Ongoing research continues to investigate the causes of psoriasis, and its triggers are still being studied. This article will outline the ways in which psoriasis compromises sleep quality, explore the potential for poor sleep to also worsen psoriasis severity, and discuss strategies to manage the skin condition and associated sleep disturbances.
What is Psoriasis?
The word psoriasis comes from the Greek roots of “psora” meaning “itch” and “-iasis” meaning “condition”.[2] As inferred from its etymology, psoriasis is a chronic condition in which a patient develops rashes with itchy, scaly patches caused by their immune system.[3] In other words, their immune system overreacts to certain triggers, causing patches throughout the body, specifically around the knees, elbows, trunk, and scalp. There are different types of psoriasis, including:[3,4,5]
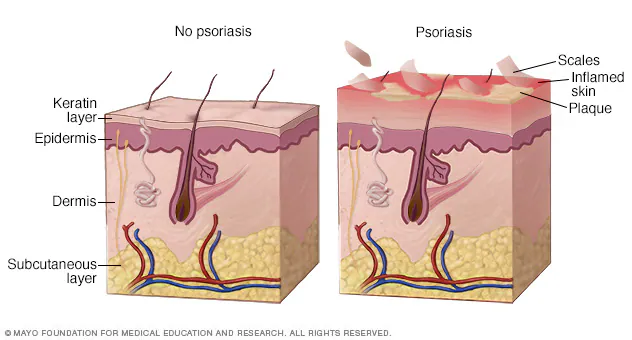
- Plaque psoriasis: This type is the most common. It looks like raised, red patches covered in white dead skin cells, and appears anywhere in the body. The white dead skin cells can look like “scales”. It can feel itchy and painful. It can be triggered by infections, weather, injuries, smoking, alcohol, and medications.
- Guttate psoriasis: This type is more common for younger individuals, such as children or young adults. It looks like small, red dots, and appears on the torso or limbs. This type is often triggered by respiratory infections.
- Pustular psoriasis: This type looks like red skin with pus-filled bumps called pustules, appearing on the hands and feet. This type has more external triggers, such as medications, infections, and certain chemicals.
- Inverse psoriasis: This type looks like smooth, red patches under areas with folds in the body, such as beneath the breasts or armpits. This type may be triggered by the constant rubbing of the skin in those areas.
- Erythrodermic psoriasis. This type is rare and severe. It looks like red, scaly skin over the majority of the skin on the body. This type may be triggered by a severe sunburn and certain medications (e.g., corticosteroids).
Although the causes of psoriasis are not fully understood, researchers have some idea of the development of the disease. It appears that psoriasis is “immune-mediated”, meaning that the immune system is over-activated to cause inflammation in the skin.[6] Additionally, genetics seems to play a part in the risk of developing psoriasis, and the heritability of the disease is above 60%.[7] As seen above, environmental and lifestyle factors may also play a part in triggering psoriasis. Poor sleep quality, for instance, is listed as one of the symptoms of psoriasis, indicating its strong linkage to sleep.[3] But how do psoriasis and sleep impact each other?
The Relationship Between Psoriasis and Sleep
As mentioned, those with psoriasis develop itchy rashes, and these rashes can make it difficult to fall asleep and can lead to nocturnal awakenings.[8] Someone suffering from psoriasis may have a flare-up as they are trying to sleep or even while they are asleep, leading to uncomfortable sensations that disrupt the natural sleep cycle. Additionally, psoriatic arthritis (a condition where the skin patches of psoriasis are accompanied by joint pain, stiffness, and swelling) can lead to further sleep fragmentation and non-restorative sleep, with some studies linking psoriatic arthritis to a greater prevalence of sleep disturbances than in cases with psoriasis alone.[8,9] While it is understandable why physical disturbances (itchiness, pain, etc.) can lead to sleep fragmentation, what is less understood is why psoriasis can actually cause sleep disorders, such as obstructive sleep apnea (OSA).

While it is estimated that 0.6-4.8% of the world’s population suffers from psoriasis, and an estimated 9-38% of the population suffers from obstructive sleep apnea, roughly 36-81.8% of those with psoriasis also suffer from OSA.[8,14] This increased prevalence of obstructive sleep apnea in those with psoriasis isn’t coincidental. The relationship between the two appears to be bidirectional; psoriasis tends to be associated with an increased risk of OSA, and OSA increases the risk of psoriasis.[10] One key factor behind this relationship is due to a shared inflammatory milieu (the “inflammatory environment” that comprises immune cells, hormones, stress signals, and cytokines, the immune system’s chemical messengers).[11,12]
Psoriasis and OSA are both chronic systemic inflammatory conditions, meaning they take place on a greater level and impact the whole body as opposed to a localized disorder, which affects just one area of the body.[11] Those with OSA have repeated drops in their oxygen level and increased sleep fragmentation, conditions that are tied to systemic inflammatory stress.[9] This stress causes increased pro-inflammatory activity, which, in an inflammatory immune pathway-driven condition like psoriasis, can cause flare-ups to become more frequent or intense.[9] This shared inflammatory pathway appears to be the best hypothesized rationale for why OSA and psoriasis can worsen each other.
Interestingly, taking care of one condition may also help improve the other. For example, smaller studies have shown that taking an anti-inflammatory treatment for psoriasis (such as TNF-𝛼 inhibitors) can improve feelings of sleepiness.[11,12] Additionally, treatment of OSA through continuous positive airway pressure (CPAP) therapy can reduce inflammatory markers (such as TNF-𝛼).[8,13] While studies have not found that CPAP can directly improve psoriasis lesions, it does provide a rationale for future studies to investigate the impact of CPAP in patients with psoriasis.
Conclusion
While we don’t yet fully understand the finer details of the relationship between psoriasis and sleep, we do know that it exists, and the inflammatory response due to poor sleep or psoriasis flare ups serve as a key mechanism. While there is reason to suspect that reducing inflammation by treating one of these has the potential to improve both, definitive research on this topic is lacking. Throughout the next few weeks, we will continue this series on sleep and the skin to better show how intricate the body really is.
No one individual is an expert in every aspect of the body, and it takes a team to manage multiple conditions impacting your sleep. Empower Sleep can help guide you to figuring out your first step towards a deep, restful night.





























































































%20thumbnail.jpg)
.png)