Reviewed by Sahil Chopra, MD, and Stacey Gunn, MD.
Research by Savit Malhotra.
Introduction
Previously, we looked at how sleep apnea and heart failure go hand-in-hand, how the two are related, and how treating one affects the other. In this week’s article, we will continue our discussion as to how sleep apnea affects the cardiovascular system with a particular focus on atrial fibrillation (AFib). AFib is just as widespread as any of the previous conditions we have discussed, and even more so in patients with sleep apnea. By the end of this article, we hope to have educated our readers on what AFib is, how it relates to sleep apnea, and what a person can do to help treat their AFib/sleep apnea.
What is Atrial Fibrillation
Atrial Fibrillation, commonly known as AFib, is when the heart beats at an irregular rhythm. This “arrhythmia” is when the upper chambers of the heart beat out of sync with the lower chambers of the heart, often beating fast and different from their normal rhythm. AFib can lead to a number of conditions, including stroke and heart failure, and people with the condition report having a fast heartbeat accompanied by shortness of breath or a feeling of light-headedness. However, the condition can often manifest itself as symptomless and can come and go.[1]
It has been estimated that AFib affects roughly 5% of the United States’ population, accounting for about ten and a half million adults, according to recent research and estimates from the University of California, San Francisco.This number is three times higher than earlier estimates, with the increase thought to be related to an older population, increased rates of high blood pressure, diabetes, and obesity, and to better detection.[2] AFib itself typically doesn’t lead to death, but the conditions that arise from AFib can.[3] Some studies have found that AFib can increase the likelihood of stroke by five times what it should be, and what is worse is that AFib-related strokes have been deemed to be more serious due to relatively more brain damage and long-term effects worse than strokes from other causes.[4] Treating AFib, and even better, preventing it, remain important courses of action for a person to take in ensuring they are able to live a long, healthy life.
How Do the Two Worsen Each Other?
Rough estimates predict that, of the patients diagnosed with AFib, half also have sleep apnea.[5] Like many of the other conditions we have discussed, the exact mechanisms behind why this is the case still remain up for debate. Many call this relationship bidirectional, but based on our research, this relationship appears to be more one-directional, with sleep apnea leading to or worsening AFib. The damage that the heart endures due to sleep apnea is one of the leading theories behind the pathophysiology of the relationship. For example, the low oxygen levels that are characteristic of sleep apnea lead to high blood pressure, rapid heart rate, and a narrowing of the blood vessels. The heart doesn’t want to be placed under this level of stress, and the body then increases its demand for oxygen. To meet this increased demand, the heart cells and tissue are remodeled and rearranged, a process known as cytoarchitectural renovation, which affects the normal functioning of the heart. This new structure and function leave the heart more susceptible to arrhythmias.[6]
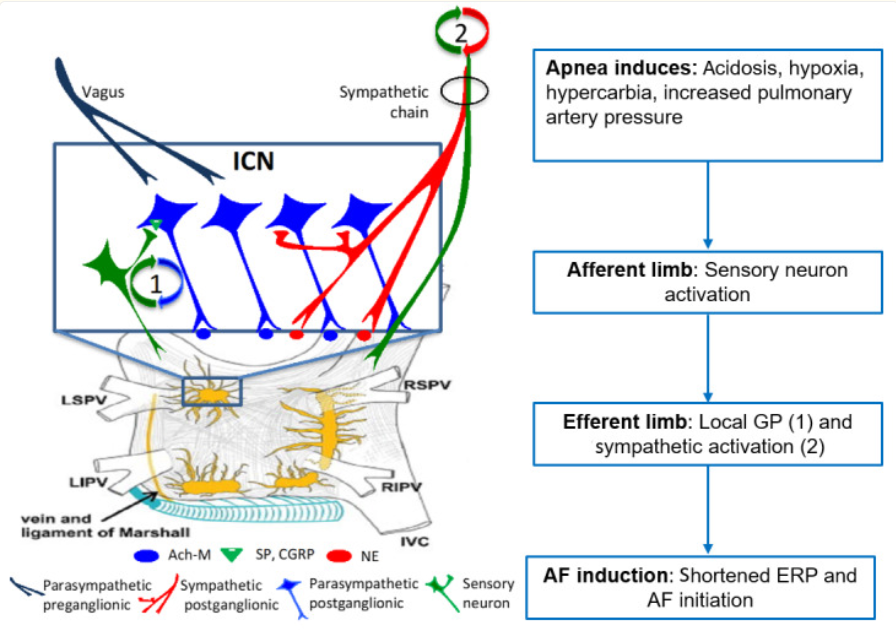
Another mechanism, and one of the more growing ideas, that could explain why sleep apnea leads to AFib, is the effect that the cardiac autonomic nervous system (ANS) has. The cardiac ANS is responsible for all processes that you cannot control, such as your heart rate, blood pressure, and more. Essentially, the theory is that apneic events cause cardiac ANS activation by first causing acidosis, increased pulmonary artery pressure, and more. In turn, this causes the sensory neuron to activate, which then activates local cells in the heart and the sympathetic nervous system (the fight or flight response). The atrial effective refractory period (ERP) is shortened, and AFib can result.[7]
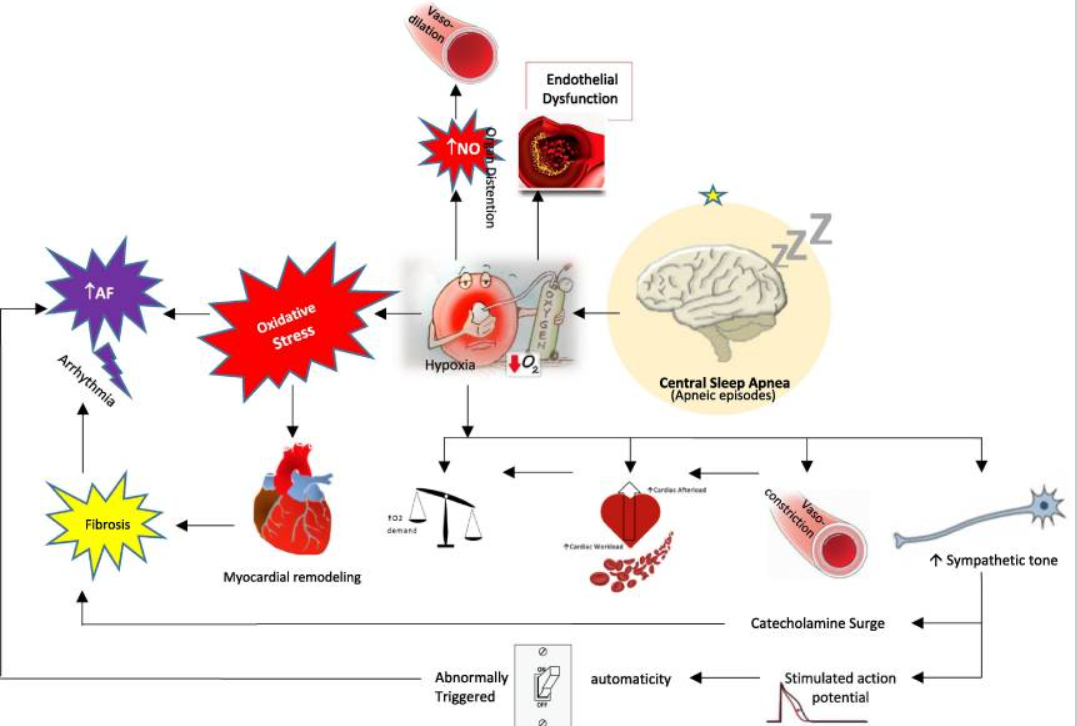
The final potential mechanism that we will be looking at relates to oxidative stress, which is when there is an imbalance of antioxidants and free radicals in your body that causes cell damage.[8] For more information on this topic, we talk in slightly more detail about oxidative stress in our article on how diabetes relates to sleep apnea. Oxidative stress occurs when the electron transport chain is disrupted due to desaturation (loss of oxygen) events that occur during sleep apnea. An increase in oxidative stress can cause mitochondrial malfunction and cellular damage, which leads to a number of other smaller changes in the body (we will not be diving too deep into the nuances here, but for more information, please see reference 8). Oxidative stress further leads to changes in the heart (like we talked about earlier), which can create a scenario where AFib is more likely to occur.[8] Furthermore, oxidative stress also leads to sympathetic nervous system activation, which we discussed is another idea behind how AFib can come about. Central sleep apnea gives rise to oxidative stress due to the decrease in oxygen levels in the blood, which can directly cause AFib or first cause myocardial remodeling (effectively the same as cytoarchitectural renovation) that leads to fibrosis (the formation of scar tissue on the organs) and then AFib.[9]
What Happens When You Treat Sleep Apnea?
Observational studies have shown that treating the sleep apnea can help keep a patient out of atrial fibrillation, although randomized trials have not borne out the same results, thought to be because the most severe cases get excluded from those types of trials. Some studies have found that, when patients treated both their sleep apnea and AFib, CPAP was effective in reducing the recurrence of AFib. This is especially true for patients who underwent catheter ablation for AFib in addition to CPAP treatment. Catheter ablation is a procedure where a catheter is inserted and used to target and destroy tissue areas of the heart that cause AFib and irregular heartbeat.[5]
Another study stated that, “Risk of recurrent AF[ib] after is diminished by OSA treatment with CPAP.” (Marulanda-Londoña et. al) This study stated that treatment with CPAP resulted in 18% of a total of 10,132 patients being hospitalized (with no increase in the risk of death due to cardiovascular disease compared to those without sleep apnea), but not treating sleep apnea was associated with an 82% chance of AFib reoccurring.[10] This study further notes that the mechanism behind why CPAP is effective in reversing AFib is not fully understood but instead theorized to be because CPAP can help reverse the structural changes in the heart that we previously discussed. At the end of the day, treating sleep apnea should be something that is done regardless of if a person has AFib or not. Doing so can help prevent a host of other diseases, and if AFib is one of those diseases, then there is no reason not to treat it.
What Should I Look Out For?
As we discussed in the previous article, the STOPBANG method remains an effective way for a person to help screen themself to see if they have sleep apnea. This test/acronym (posted below for reference) isn’t perfect, but it is still an incredibly useful tool.
- S - Snoring
- T - Tiredness during the day
- O - Obstruction (brief pause in breathing while sleeping)
- P - Pressure (high blood pressure)
- B - Body mass index of 30 or greater
- A - Age of 50+
- N - Neck circumference of greater than 16 inches (in women) or 17 inches (in men)
- G - Gender (male)
If you have three or more of the above-mentioned characteristics of sleep apnea, it is important that you see a sleep medicine doctor so that they can properly diagnose you and you can begin treatment. Although, we will also mention that it is possible to have sleep apnea even with a low STOPBANG score, and so a normal score should not prevent someone from being evaluated if they are otherwise concerned.[11]
As for AFib, while we mentioned earlier that it can present itself as symptomless, there are still a number of signs to look out for. Palpitations (fast, fluttering feelings in the heart), pain in the chest, fatigue, lightheadedness, dizziness, shortness of breath, weakness, and a reduced ability to exercise are all among the potential symptoms. Additionally, AFib can present itself occasionally, persistently, or permanently.[1] If you believe you may have AFib, or are worried about any other condition, it is important to see a doctor immediately, and if it is an emergency, please call 911.
Conclusion
We have spent the last few articles diving into how sleep apnea affects the heart, and for good reason. The number of different impacts that sleep apnea has on the cardiovascular system warrants attention, and although we may not fully understand the relationship, we know enough to say that there is a correlation between the heart and sleep apnea. Oftentimes, people notice problems in either their breathing or their heart health and decide that they are fine without getting any proper medical attention. The facts are simple: Sleep apnea can greatly impact your day-to-day life and lead to the development of heart-related illnesses, and ignoring signs pointing to this can lead to tragic results, including death. While sleep apnea itself is a rare cause of death, the impacts it has on the body are lengthy, and many of the conditions that are caused by sleep apnea can lead to death. Next week, we will begin looking at how sleep apnea impacts the brain, with a focus on dementia.






























































































%20thumbnail.jpg)
.png)