Reviewed by Sahil Chopra, MD, and Stacey Gunn, MD.
Research by Savit Malhotra.
Introduction
In the previous article, we did an in-depth look at the relationship between coronary artery disease (CAD) and sleep apnea. In this entry, we established the role that sleep apnea plays in heart disease, if CPAP can help prevent your risk of developing heart disease, and signs to look out for. This week, we will continue looking at the relationship that sleep apnea has with the cardiovascular system, focusing specifically on heart failure. This is a serious condition that can share a bidirectional relationship with sleep apnea, but due to limitations in research, the full extent of the relationship is not entirely clear. However, current research has established a clear link between the two, which we will share shortly.
What is Heart Failure?
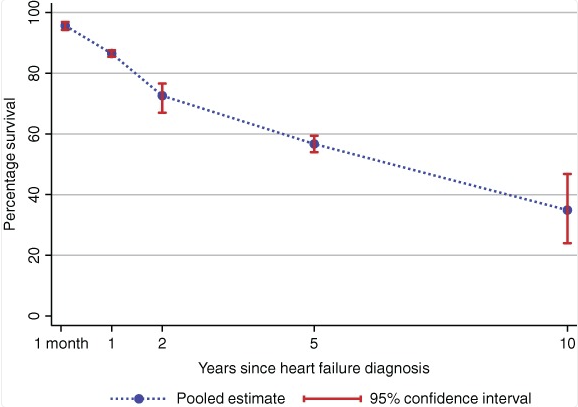
Heart failure, also known as congestive heart failure, is a chronic condition that impacts how the heart pumps blood throughout the body. Over time, the heart becomes weaker and weaker and is unable to pump blood at a normal rate, causing the blood to pool in the lungs and legs.[1] Due to the body’s blood needs not being met, heart failure can be life-threatening and can become life-ending. The heart can continue to weaken over time, so much so that the body is no longer able to compensate for the weakened flow of blood.[2] Survival rate tends to worsen over time, with the 1-year survival rate of 86.5% dropping to 72.6% after another year, then 56.7% 3 years later, and 34.9% 5 years later (1-year, 2-year, 5-year, and 10-year survival rates).[3]
It is important to note that heart failure is not the same as cardiac arrest, where the heart stops working altogether, although each can cause the other. In patients with heart failure and weakening of the muscle, there is an increased risk of abnormal heart rhythms which can cause the heart to stop (or arrest). Conversely, patients who have coronary artery disease and suffer from a heart attack can potentially go into cardiac arrest, and may be left after that episode with a weakened heart due to muscle damage. [4] Heart failure is a common disease in the United States, with about 6.7 million adults (20 years or older) having the condition and 452,573 having passed due to heart failure in 2023 (this accounts for 14.6% of all deaths in 2023).[5]
How Do the Two Worsen Each Other?
One article estimates that those with sleep apnea have a 140% increased risk of heart failure.[7] A different study found that those with the worst obstructive sleep apnea (measured as those in the highest quartile of apnea-hypopnea index) were 2.38 times more likely to have heart failure.[8] There are two main reasons that heart failure and sleep apnea are associated: stress to the nervous system (via sympathetic nervous system activation and vagal withdrawal) and a change in blood flow/blood oxygen levels.[9] Beginning with stress to the nervous system, this occurs due to sleep apnea activating the fight-or-flight response (sympathetic nervous system activation), and when activity of the vagus nerve (which is the cranial nerve responsible for the heart) is reduced. When the fight-or-flight response is activated, the heart has to pump more blood in order to fuel the body with more oxygen, putting more wear and tear on the heart.[10] Sleep apnea has been known to activate the fight-or-flight response over and over again during sleep, which is unnecessary and only puts more stress on the brain and the heart.[11] This stress to the heart is further worsened by vagal withdrawal during sleep apnea. Essentially, those with sleep apnea experience impaired vagal activity, which means the heart is not properly regulated.[12] In terms of a change in blood flow/blood oxygen level, those with sleep apnea may experience low oxygen levels in their blood and high blood pressure. As a result, the cells in the heart can become damaged, leading to heart failure. Over time, the repeated stress created by the sleep apnea leads to a worsening of symptoms, and even death.[13]
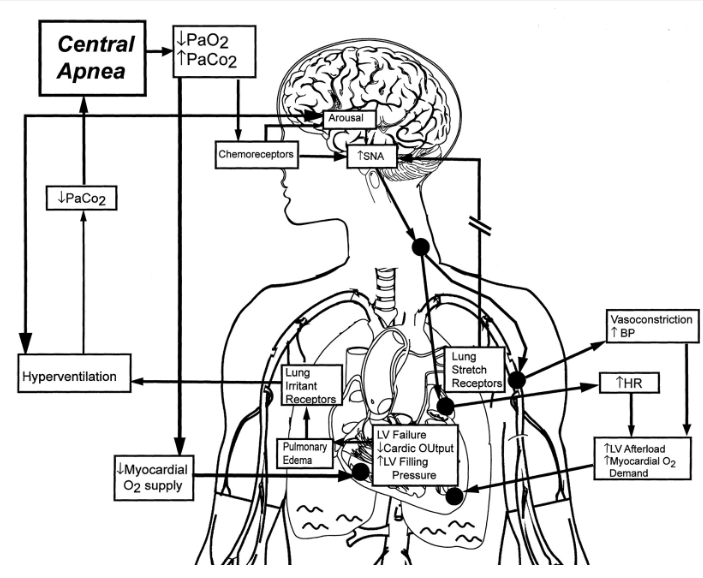
It has also been found that sleep-disordered breathing is fairly common in those with heart failure, and that those with reduced ejection fraction have an increased risk of central sleep apnea, while those with heart failure with preserved ejection fraction have an increased risk of obstructive sleep apnea.[14] In heart failure, the pressure in the left ventricle during its filling phase (diastole) rises, leading to fluid buildup in the lungs. This fluid buildup stimulates receptors in the lungs that signal the brain to increase breathing, resulting in over-breathing, or hyperventilation. This excessive ventilation lowers carbon dioxide (CO2) levels in the blood. Because CO₂ plays a key role in regulating the drive to breathe, when its level drops too low, the brain may temporarily stop sending signals to breathe, causing central sleep apnea. If this occurs during sleep, the person may briefly wake up (an arousal), triggering a burst of rapid breathing, which can further reduce CO2 levels and set the stage for the next apnea. This cycle can repeat throughout the night.[9]
What Happens When I Treat My Heart Failure or Sleep Apnea?
It has been shown that, by treating heart failure, patients can experience an improvement in their central sleep apnea. Specifically, current literature supports the idea of non-pharmacological therapies being equally important as pharmacological ones. These treatments include cardiac resynchronization therapy, atrial overdrive pacing, and cardiac transplant.[15] The aforementioned article also notes that medications are equally important in the treatment of central sleep apnea by means of treating heart failure, and combined with the non-pharmacological remedies, a person is able to optimally treat their heart disease. What has also been discovered is that, when you treat sleep apnea with CPAP in patients with heart failure, there is a reduction in blood pressure and heart rate during sleep and hypoxia (when the body doesn’t get enough oxygen).[16] By reducing the stress on the cardiovascular system, the hope is that you should be able to lower your risk of heart failure and heart disease as a whole. Furthermore, treating congestive heart failure can help with redistributing fluid that contributes to crowding in the airway, thereby sometimes helping with obstructive sleep apnea. However, this doesn’t eliminate the apnea entirely.[17]
In terms of heart failure, one study found that after CPAP was used for 1 month, left ventricular ejection fraction (essentially how much blood the heart’s left ventricle is able to pump out) increased by 12%, from 37% to 49%, and then reversed after just 1 week of CPAP withdrawal. In the eight patients who were included in this study, their dyspnea (shortness of breath/uncomfortable breathing) was also reduced.[18] While this study was uncontrolled, a similar, controlled study showed that 12 patients placed randomly into a test group with 1 month of CPAP usage experienced a 9% increase in left ventricular ejection fraction while the control group experienced no improvement.[19] Evidence has also shown that by treating sleep apnea, some of the symptoms of heart failure can be reduced, and quality of life can be improved. What has yet to be uncovered, however, is that there is a reduction in hospitalizations or mortality.[20] Although there are still some uncertainties, the current data paints a clear picture: there is definitely a benefit to treating both conditions.
What Should I Look Out For?
Those who have already been diagnosed with sleep apnea or heart failure should closely monitor their symptoms and conditions and be aware of any worsening of either. Those who have not been diagnosed with sleep apnea can use the following test/acronym to determine if they should see a doctor: STOPBANG[21]
- S - Snoring
- T - Tiredness during the day
- O - Obstruction (brief pause in breathing while sleeping)
- P - Pressure (high blood pressure)
- B - Body mass index of 30 or greater
- A - Age of 50+
- N - Neck circumference of greater than 16 inches (in women) or 17 inches (in men)
- G - Gender (male)
If you have three or more of the above-mentioned characteristics of sleep apnea, it is important that you see a sleep medicine doctor so that they can properly diagnose you and you can begin treatment. Although, we will also mention that it is possible to have sleep apnea even with a low STOPBANG score, and so a normal score should not prevent someone from being evaluated if they are otherwise concerned.
As for heart failure, there are a number of symptoms here that you should be on the lookout for. These symptoms include shortness of breath, coughing or wheezing that is persistent, edema (swelling caused by increased fluid buildup), tiredness, lack of appetite, fatigue, impaired thinking, increased heart rate, and weight changes.[22] Keeping track of your body and any changes to it is the best course of action for most medical problems, and keeping a record of these changes can help you during later diagnosis. If you ever become concerned that you are experiencing an immediate medical problem, such as a heart attack, please call 911. If any of the symptoms become problematic in your daily life, consult with a physician so that they may help you with any issues.
Conclusion
Sleep apnea and the heart go hand in hand, and any evidence of heart failure or sleep apnea should be taken seriously. It is not uncommon for people to think they may have sleep apnea and not seek treatment because they don’t think it will greatly impact them. This is simply not the case. Sleep apnea can give way to serious cardiovascular problems, and any evidence suggesting sleep apnea should be taken seriously. Similarly, any evidence of heart failure in and of itself is problematic, and those with heart failure should be aware of their increased risk of sleep apnea. The development or worsening of either condition should be noted, and a doctor should be consulted when these symptoms arise. The team and Empower Sleep want to make sure you live a long, healthy life, and this begins with educating our readers on the dangers of sleep apnea and other related diseases. If you are worried that you may have sleep apnea, please contact us so that our care team can further assist you, or see your primary physician for recommendations on next steps.






























































































%20thumbnail.jpg)
.png)