Reviewed by Sahil Chopra, MD, and Stacey Gunn, MD.
Research by Savit Malhotra and Theresa Do.
Introduction
For our final installment of the skin and sleep series, we will discuss a topic that can pop up in our lives. This condition is highly prevalent during adolescence and early adulthood. It affects around 85% of those who are ages 12 to 24.[1] If you thought of “acne”, then you are correct! Acne vulgaris, also known more simply as acne, is one of the most common skin disorders. Outside of its skin effects, acne can also contribute to a lack of confidence, anxiety, and depression.[2] This blog will extract information about the condition, including its symptoms and treatments. We will also dive into research on how sleep and acne are connected.
What is Acne
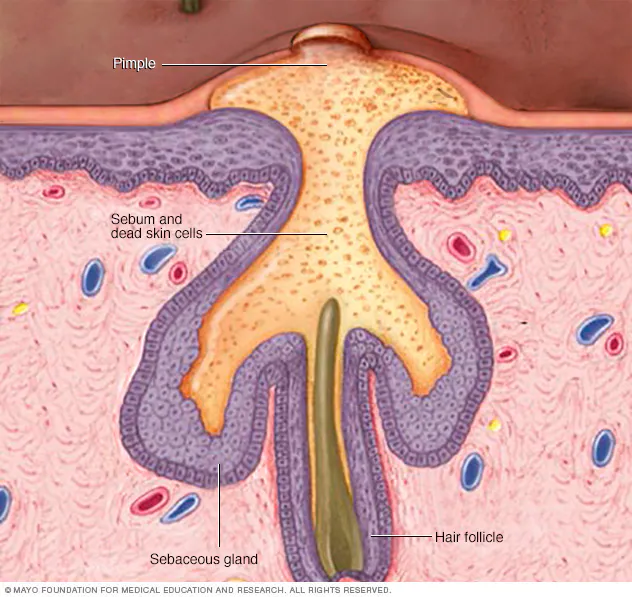
Acne is a skin condition that clogs your hair follicles, creating pimples, whiteheads, and blackheads.[3,4] The illustration below briefly shows how a pimple is formed. It is important to note that although most concerns are aimed towards facial acne, acne can occur anywhere on the body. Sebum, or skin oil, is naturally occurring through our sebaceous glands. It functions as a barrier against environmental damage and microbial infections. When there is an overproduction of sebum, it can mix with dead skin cells and bacteria on your skin to clog hair follicles. Triggers of sebum overproduction include hormone changes, stress, certain medications, and diet.
There is a scale of acne types, ranging from whiteheads to cystic lesions.[3,4] Whiteheads (closed comedones) are closed, plugged pores. They appear as small white bumps that are still underneath the skin. When the bump is exposed to the air through the top layer of skin being opened up, whiteheads can become blackheads (open comedones) from the oxidation of the sebum-bacteria-dead skin mixture. Blackheads are not from dirt, as is commonly misunderstood. Acne can become inflamed, and the pore can burst, turning into pimples with pus. Pus is a liquid generated from white blood cells fighting against bacteria. In more severe cases of acne, pimples become painful cysts (pus-filled lumps under the skin) or nodules (large lumps under the skin). Both types can lead to scarring and skin discoloration.
Acne treatments can be either topical or oral, depending on the type of acne and the severity.[5] A dermatologist typically assesses this through a physical examination of your skin. They will see whether your acne is open/closed as well as the level of inflammation. They will also assess your current skincare routine to see whether it is appropriate for your skin type and needs. The first line of treatment often includes topical treatments, including topical retinoids and topical antimicrobial agents. Topical retinoids, such as tretinoin, adapalene, and tazarotene, work by targeting the skin’s inflammatory response. Retinoid is a Vitamin A derivative known to target skin aging and improve skin turnover.[5,6] These treatments can help the skin heal from acne. Topical antimicrobial agents, such as benzoyl peroxide, clindamycin, and erythromycin, are used to prevent the overgrowth of bacteria on the skin. Cutibacterium acnes (C. acnes), or Propionibacterium acnes (P. acnes), are closely connected to acne because they live in/on the skin and thrive off of sebum.[7] When excess sebum is secreted or triggered, there can be a growth of these bacteria, leading the inflammation response in the pores. Topical antimicrobial agents kill or inhibit the growth of these bacteria.
Supportive therapy includes modifying lifestyle and skincare habits. In general, a patient is encouraged to wash their face twice daily using gentle skin products and avoiding scrubbing or exfoliating. For those who use makeup, “noncomedogenic” and “oil-free” products can help limit further skin irritations. Using sunscreen is also strongly recommended, as it can prevent further skin damage and pigmentation. [1,5]
In more serious cases of acne, topical treatments may not be enough. Doctors may prescribe oral treatments to combat acne. This includes systemic antibiotics, isotretinoin, and hormonal therapies.[5] With these oral medications, the aim is to gain control of the inflammation while targeting the causes. These treatments oftentimes require close monitoring due to risks and side effects. Systemic antibiotics not only reduce the concentration of C. acnes but also reduce inflammation. The concern with systemic antibiotics includes antibiotic resistance. Therefore, these treatments are limited to a duration of no more than 3 to 4 months. Additionally, oral antibiotics are recommended to be combined with benzoyl peroxide and topical retinoids.[8] If other therapies do not work, then isotretinoin may be prescribed. Isotretinoin, commercially known as Accutane, works by reducing sebum production throughout the body. This, in turn, also reduces the concentration of C. acnes and inflammation. In the past, Isotretinoin had been linked to depression and suicide, and, therefore, those on the medication would often be required to have follow-up appointments. However, later large-scale evidence showed that this didn’t pan out at the population level. In fact, the rates of depression and suicidality were lower in patients who were being treated with isotretinoin. This is thought to be because of less social stigma surrounding the treatment.[9] Lastly, hormone therapies, like oral contraceptive pills, can help manage acne through stabilizing hormone fluctuations for women. The fluctuation of hormones can lead to changing levels of sebum and, therefore, various pimples throughout the menstrual cycle.[10] As always, we recommend consulting with your doctor regarding which dermatologic treatment may be best for you.
Sleep and Acne
Several studies have found that poor sleep quality (as indicated by high Pittsburgh Sleep Quality Index scores) is associated with significantly greater acne severity in adults.[11,12,13] This link is primarily driven by periods of sleep deprivation, as people with acne report shorter sleep duration and subjectively worse sleep quality compared to those without acne.[11] It has been noted that sleep deprivation results in hormonal imbalance, immune dysregulation, and increased inflammation, all of which can result in acne flares.[11,12] One key mechanism behind this relationship is the increase in cortisol levels resulting from a poor night of sleep.[11] Cortisol, the body’s stress hormone, helps to regulate sebaceous glands (oil glands). Increased cortisol levels result in increased activity of this gland (known as sebaceous activity), causing the body to produce more sebum (skin oil).[14] The increase in sebum secretion has been shown to worsen acne lesions. Aside from cortisol, poor sleep has also been associated with increased pro-inflammatory cytokines (namely IL-6 and TNF-⍺) and substance P, both of which also promote sebaceous activity and inflammation.[12] Aside from causing acne, poor sleep can also make treatment less effective. It has shown that worse sleep quality can lead to poorer outcomes after laser therapy for acne scars, as well as increased transepidermal water loss, which can impair the skin barrier’s activity to recover.[12]

Interestingly, sleep and acne have a bidirectional relationship, meaning that acne can actually worsen your sleep quality. Acne is often associated with negative self-perception of appearance, with individuals with acne reporting reduced satisfaction with their physical appearance compared to those without acne. These negative perceptions can lead to increased psychological distress, contributing to insomnia, anxiety, and depression, all of which negatively affect sleep quality.[12] One study also notes that acne severity is associated with lower dermatology-related quality of life, which independently predicts poorer sleep quality.[11]
Conclusion
Acne is a very common condition, affecting individuals from adolescence through adulthood, and sleep plays an important (and often overlooked) role in its severity. Poor sleep can worsen acne by increasing stress hormones and inflammation, leading to more frequent or severe breakouts. In turn, this acne can negatively impact self-perceptions, increasing nighttime stress and making it difficult to fall or stay asleep. Together, this creates a self-reinforcing cycle of poor sleep and acne that perpetuates one another.
Breaking this cycle requires addressing both skin health and sleep health, and the Empower Sleep team is here to help with the latter. While acne treatments like topical creams and systemic therapies can target the underlying factors of acne, poor sleep might lead to these treatments having suboptimal effects. Our care team is well-versed in addressing all underlying factors of poor sleep, including stress and disrupted sleep routines. By tackling these factors, you’ll be able to make an impact on both your skin health and your overall wellness.





























































































%20thumbnail.jpg)
.png)